Simulation-based team training in obstetrics

The study of Annemarie Fransen and her team shows that simulation-based team training is effective in improving communication and cooperation of obstetric care teams.
Posted by
Published on
Thu 01 Nov. 2018
Topics
| Medical Encounter | Medical Simulation | Simulation-based Training | Team Training | Teamwork | TrackLab | Viso | Healthcare |
The author of this guest blog post, Annemarie Fransen of the Máxima Medical Center in Veldhoven, The Netherlands, focused in her PhD thesis on the development and evaluation of simulation-based team training in obstetrics. Her research shows that simulation-based team training is effective in improving communication and cooperation of obstetric care teams.
Obstetric care is characterized by life threatening events that can happen at any moment. The quality of obstetric care is influenced by the quality of teamwork performance of the involved care teams. Unfortunately, this team performance is not always optimal, and in 75% of medical errors there is a relation with a lack of teamwork skills and/or communication.
These medical errors can lead to serious morbidity and mortality for mothers and their babies. In order to reduce the number of medical errors, training of healthcare teams by using simulation-based medical education is proposed. This blog is about the effect of simulation-based obstetric team training on teamwork performance and patient outcome.
Teamwork skills
Teamwork skills are defined as behaviors that facilitate effective team member interaction (Beaubien et al, 2004). It includes skills like leadership, communication, situational awareness, and decision-making. Being educated in these skills is necessary and can be provided by the use of simulation-based team training. Evaluation of team training showed better capabilities for dealing with fatigue, teambuilding, communication, recognition of dangerous situations, and decision-making (Grogan et al, 2004).
Also in obstetrics, simulation-based team training programs have demonstrated positive effects on trainees’ attitude, perception of performance, knowledge, clinical management, and task completion (Robertson et al., 2008; Birch et al., 2007; Daniels et al., 2010). There was also an association with positive effects on patient outcome (Draycott et al, 2006). However, most of these trials were non-randomized studies, and a comparison with no intervention was missing.
For this reason, we initiated a randomized trial, evaluating the effect of simulation-based obstetric team training on teamwork performance and patient outcome.
Debriefing simulation training
We performed a large cluster-randomized controlled trial that evaluated the effect of simulation-based obstetric team training (Fransen et al., 2012; Fransen et al., 2017). In total, 24 Dutch hospitals were included, of which the complete obstetric department participated in the study. After randomization, 12 hospitals received the intervention and 12 hospitals received no intervention.
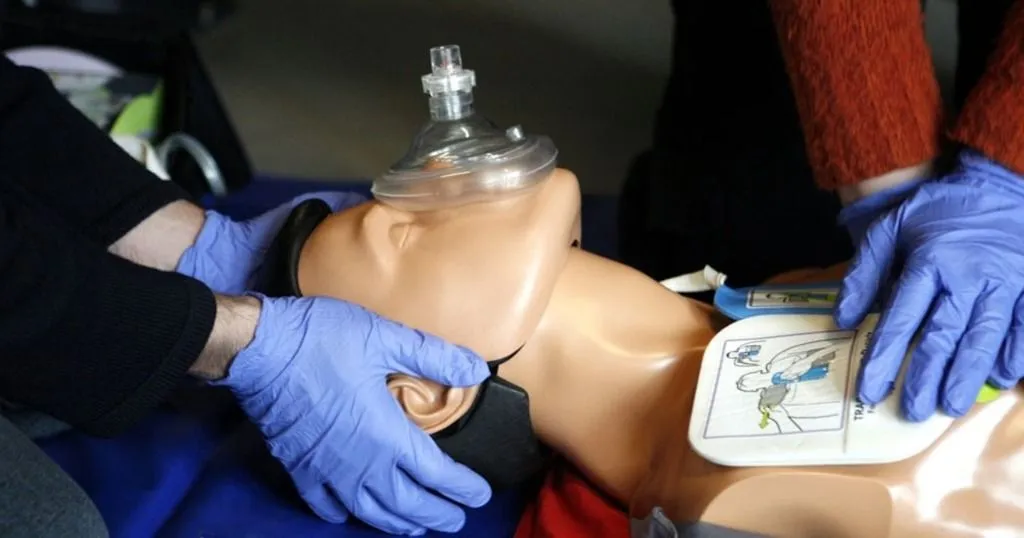
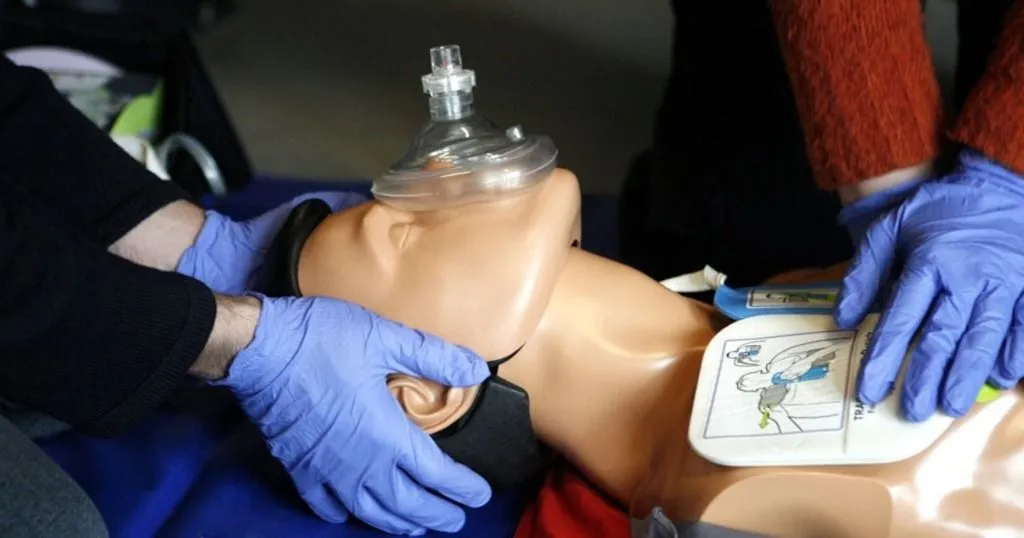
The intervention comprised a one-day, multi-professional, simulation-based obstetric team training that was provided in a medical simulation center. In total, 74 multi-professional teams, including 471 trainees, received the intervention. The multi-professional teams had to manage five simulated obstetric emergencies. Each scenario lasted approximately 15 minutes, and was videotaped.
The video recordings were used to provide feedback on teamwork and medical technical skills. This debriefing was provided after each scenario by a medical specialist and communication expert. We mainly focused on the education of teamwork skills.
Effect on teamwork performance and patient outcome
Approximately 6-8 months after the intervention, we visited all included hospitals to measure the effect on teamwork performance. This was done by performing two unannounced in situ simulations on their delivery rooms. The team on call had to manage a shoulder dystocia. The second scenario comprised the resuscitation of a pregnant woman. To measure teamwork performance, we used the Clinical Teamwork Scale (Guise et al. 2008).
The teams from the intervention groups showed better results on the Clinical Teamwork Scale. Besides, they used predefined essential medical skills more often, in comparison to the teams in the control group.
All included hospitals registered 5 obstetric complications during a one year follow-up. These complications included: low Apgar score after 5 minutes, postpartum hemorrhage, trauma due to shoulder dystocia, eclampsia, and hypoxic-ischemic encephalopathy. After one year, there was no difference between study groups in the combined outcome measure that included the obstetric complications described above.
However, we did found a lower number of trauma due to shoulder dystocia in the intervention group. Moreover, the intervention group used more frequently invasive treatment options for severe postpartum hemorrhage, which was advised during the training course.
Future research
In order to increase the effectiveness of simulation-based obstetric team training courses, team behaviors need to be explored. In cooperation with Noldus Information Technology, we performed a pilot study to investigate the walking behavior of team members. Two patient actors, using a birthing simulator, imitated two obstetric scenarios.
Each scenario was performed twice (with intermittent feedback) by a novice leader together with both an experienced and unexperienced nurse. The same scenarios were performed once by an expert team comprising of an expert leader (obstetrician with > 15 year experience in a Dutch perinatal center) and two experienced obstetric nurses.
Movements were visualized and analyzed by TracklabTM. Their software enabled us to calculate the relative walking time (the absolute time the participant was moving divided by the absolute time the participant participating in the scenario), and to generate a heat map (an overview of how much time a leader spent at a location).
Interested in human behavior research? Read more on 'How to study human behavior'!
References
- Beaubien JM, Baker DP. The use of simulation for training teamwork skills in health care: How low can you go? Qual Saf Health Care. 2004;13:i51-6.
- Birch L, Jones N, Doyle PM, et al. Obstetric skills drills: evaluation of teaching methods. Nurse Educ Today. 2007;27:915-22.
- Daniels K., Arafeh J., Clark A., Waller S., Druzin M., Chueh J. Prospective randomized trial of simulation versus didactic teaching for obstetrical emergencies. Simul Healthc. 2010;5:40-5.
- Draycott T, Sibanda T, Owen L, et al. Does training in obstetric emergencies improve neonatal outcome? BJOG 2006;113:177-82.
- Fransen AF, Ven van de J, Merién AER, De Wit-Zuurendonk LD, et al. Effect of obstetric team training on team performance and medical technical skills: a randomised controlled trial. BJOG 2012;119:1387-93.
- Fransen AF, van de Ven J, Schuit E, van Tetering A, Mol BW, Oei SG. Simulation-based team training for multiprofessional obstetric care teams to improve patient outcome: A multicentre, cluster randomised controlled trial. BJOG. 2017;124:641-650.
Related Posts
Evaluating ergonomics in healthcare – paramedics
How to assess medical team effectiveness

