What is a placebo? And how does it work?

The placebo effect reveals how belief alone can influence pain and symptoms. Recent research uncovers brain mechanisms, like the panacea effect, involved in this effect in mice
Posted by
Published on
Tue 20 Aug. 2024
Topics
| EthoVision XT | Health Effects | Healthcare | Behavioral Research |
The placebo effect is one of the most intriguing and mysterious phenomena in both medicine and psychology. At its core, it's the ability of a person's belief or expectation to influence physical and mental health outcomes, even when no active medication is involved. While it may seem almost magical, the placebo effect is backed by significant research and plays a crucial role in how we experience pain, fatigue, and other symptoms. But how exactly does this work, and what does recent research reveal about the underlying mechanisms in the brain? Let’s dive into the science behind this fascinating phenomenon.
What is a placebo?
If someone that you trust gives you a pill and tells you that it will make your headache go away, then it helps. Even if there is no painkiller in the pill. That is the completely bizarre phenomenon that we know of as the placebo effect. It typically affects symptoms like pain, fatigue and depression and can increase or decrease the effects of drugs. And has also been found to work extremely well in the case of sea-sickness!
Dopamine
The placebo effect only works if you expect it to, hence the importance of trusting the person who administers it. Some people are genetically more predisposed to placebos than others, apparently related to dopamine levels in the brain. Dopamine is a neurotransmitter which plays a role in motivation and reward-related behavior. Personality traits also play a role in how strong the placebo effect is.
Side-effects
You can even get negative side effects like headaches or dizziness from placebos. That is called the nocebo effect. Placebo effects are so strong that in any medical trial, it is necessary to give the control group a placebo (not just an absence of treatment) so that the researchers can distinguish between the effects of the treatment being studied and the placebo effect. Sometimes people talk as if placebo effects are imaginary, ‘it is just in the mind’, but our entire experience of the world is in our minds, we know no other reality.
Double blinding
Even if the researchers know which treatments are with drugs and which are placebos (and the participants are not told), that can still have an effect. For that reason, trials are normally double-blind, so that neither the people administering the treatment, nor the subjects know which treatment they receive.
Physicians also prescribe placebos
In one survey [1], 77% of UK physicians said that they prescribed placebos at least once a week. That was mostly not a pure placebo (like a sugar pill) but one with an active ingredient, like vitamins or antibiotic for a viral disease, but which would have no biological effect on the disease in question.
Various studies [2] have shown that up to 50% of the effects of some treatments for diseases like bipolar, insomnia and depression can be due to the placebo effects. But it is not only diseases of the brain that can be affected, also cardiology, dermatology, Crohn’s disease, and urology are all areas where the placebo effect has been demonstrated, albeit sometimes with smaller effects. It is also sometimes suggested that the benefits of homeopathic medicine can be partly due to the placebo effect.

Placebos in research
Most research on placebos has been on their effects on pain (‘placebo analgesia’), but until recently, there was still not so much known about the mechanisms in the brain that caused it. However, a new study (published in 2024 [3]) has at last unravelled some of the biological mechanisms behind the phenomenon.
Behavioral experiment
A study by Chen and colleagues [3] designed an experiment in mice to investigate how the placebo effect operates in the brain. They used heated floor plates set to 48°C, which caused mild pain to the mice without causing any harm. Next to the hot plate, they placed a cooler plate at 30°C. The mice quickly learned that moving to the cooler plate would relieve their discomfort, and their movements were tracked using EthoVision XT software. Interestingly, even when the temperature of the hot floor was lowered back to 30°C, the mice still preferred the plate they had learned was cooler. This behavior mirrors the way humans trust the person administering a placebo, showing how expectation alone can influence perception and behavior.
When on the hot plate, the mice displayed behaviors to alleviate their discomfort, such as jumping and licking their paws. Remarkably, when both plates were heated to the same 48°C, the mice still preferred the previously cooler plate and exhibited fewer pain-relief behaviors. This demonstrated that the mice had developed a learned expectation of relief—similar to the placebo effect in humans. To further confirm that this was indeed a placebo-like response, the researchers performed additional tests.
To better understand the underlying brain mechanisms, the researchers mounted tiny microscopes on the mice's heads to observe brain activity during the experiment. They discovered that a specific brain region called the pontine nucleus, typically associated with controlling body movements, was highly active during the placebo effect. When the researchers turned off neurons in this area, the placebo effect vanished, indicating its crucial role in pain relief expectations.
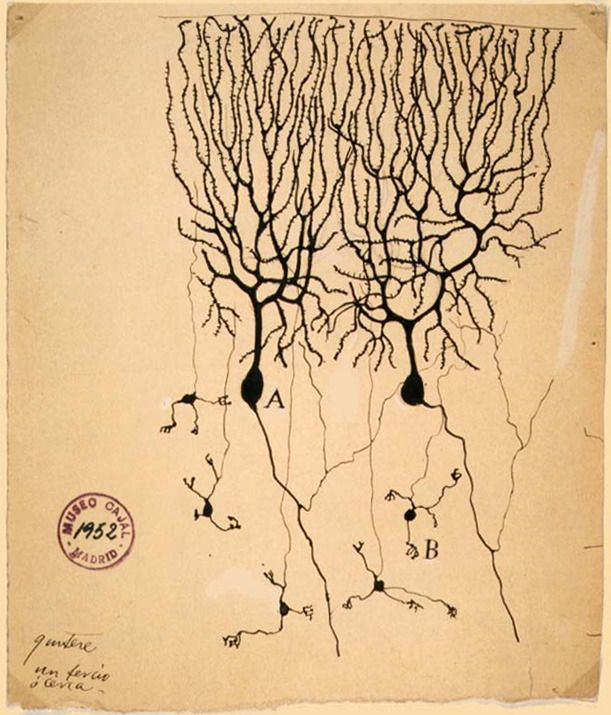
Purkinje cells
Digging deeper, the researchers identified Purkinje cells in the pontine nucleus as the specific cells responsible for encoding the expectation of pain relief (i.e., the panacea brain mechanism). Purkinje cells, are the second-largest cells in the brain, with a long axon and many branched ends (called dendrites), and are vital for coordinating motor activity and are known to have receptors for natural opioids produced by the body. Painkillers work by stimulating these opioid systems, and the research suggests that these same cells are involved in the brain's response to placebo-induced pain relief.
Two key insights
This research uncovers two key insights.
- First, it reveals that the panacea brain mechanism—the process by which the brain produces pain relief in response to the expectation of relief—operates in a way that parallels how actual painkillers work. Specifically, the placebo effect triggers the brain's opioid system, much like a drug would, leading to real pain reduction. This mechanism involves areas such as the pontine nucleus and Purkinje cells, which are key players in controlling motor functions and processing the brain’s natural opioid responses.
- Second, while the panacea brain mechanism shares similarities with how painkillers function, it also has unique elements. These differences suggest that the brain has alternative pathways to manage pain, beyond what current drugs target. Understanding these distinct pathways opens up the potential for developing new types of pain therapies that might be more effective by tapping into these specific placebo-related brain mechanisms. In essence, this research not only validates the power of the placebo effect but also points toward future innovations in pain management.
References
- Howick J, Bishop FL, Heneghan C, Wolstenholme J, Stevens S, Hobbs FD, Lewith G. Placebo use in the United Kingdom: results from a national survey of primary care practitioners. PLoS ONE. 2013;8:e58247. doi: 10.1371/journal.pone.0058247.
- Pardo-Cabello AJ, Manzano-Gamero V, Puche-Cañas E. Placebo: a brief updated review. Naunyn Schmiedebergs Arch Pharmacol. 2022 Nov;395(11):1343-1356. doi: 10.1007/s00210-022-02280-w. Epub 2022 Aug 9. PMID: 35943515; PMCID: PMC9361274.
- Chen, C., Niehaus, J.K., Dinc, F. et al. Neural circuit basis of placebo pain relief. Nature (2024). https://doi.org/10.1038/s41586-024-07816-z
Related Posts

5 proven ways to measure spatial learning in rodents

WHY use a Y-maze? Automating learning and memory tests in rodents

