Our gut microbiota influences how we feel
Our guts are our second brain. But how does that work? Researchers implanted the gut flora of depressed mice into non-depressed mice and observed the results.
Posted by
Published on
Wed 18 Sep. 2024
Topics
| Brain Research | Depression | EthoVision XT |
For a long time, we believed that the brain was the sole commander of the body, sending out instructions while receiving minimal feedback, such as signals like pain. However, recent research has flipped this notion on its head. We now know that communication between the brain and the gut is much more complex, and even more surprising—the gut has a profound influence on the brain. In fact, the digestive system not only sends signals about fullness (satiety) but also plays a crucial role in regulating our mood and behavior.
The Gut: Your "second brain"
Scientists have begun to understand the vast role the digestive system, and the bacteria living in it, plays in our overall health and well-being. The gut's influence on mood and behavior is so significant that it's often referred to as a "second brain." Although it’s been clear that the gut impacts our mental state, the exact mechanism of this communication remained elusive, until recently.
Experimental setup: Uncovering the Gut-Brain connection
To investigate how the gut affects brain function, researcher Eleni Siopi and her team conducted an intriguing experiment [1] using three groups of mice:
- A control group of socially housed, undisturbed mice.
- A group exposed to long-term mild stress.
- A group that received a fecal transplant from the stressed mice, thus inheriting the stressed mice’s gut bacteria.
Interestingly, the third group wasn’t exposed to stress themselves, but simply had gut bacteria from the stressed mice.
Unpredictable chronic mild stress
The stressed group of mice endured "unpredictable chronic mild stress" over eight weeks. This meant two stressful events each day, randomized and mild, like exposure to predator scents, cage shaking, or wet bedding. While these stressors mimic what wild mice would experience, they were delivered at a higher frequency, which typically leads to depression-like behaviors in captive mice.
A deep dive into anxiety testing
To measure the impact of stress on behavior, the researchers used a battery of behavioral tests. These tests, recorded using EthoVision XT, included:
- Open Field Test: Anxious mice explore open spaces less.
- Elevated Plus Maze: Anxious mice prefer closed arms with high walls over open, exposed arms.
- Light and Dark Box Test: Mice prone to anxiety spend more time in the dark.
- Sucrose Preference Test: Depressed mice show less interest in sweetened water.
- Novelty Suppressed Feeding Test: Anxious mice hesitate to retrieve food in brightly lit environments.
- Tail Suspension Test: Depressed mice stop struggling sooner when suspended by their tail.
- Forced Swim Test: Similarly, depressed mice give up trying to escape when placed in water.
Key findings: Stress in the Gut, stress in the brain
The stressed mice exhibited behaviors typical of depression across these tests, which was expected. However, the mice that had received fecal transplants from stressed mice also displayed the same depression-like symptoms, despite not being stressed themselves. This suggests that signals originating in the gut were being sent to the brain, triggering these behaviors.
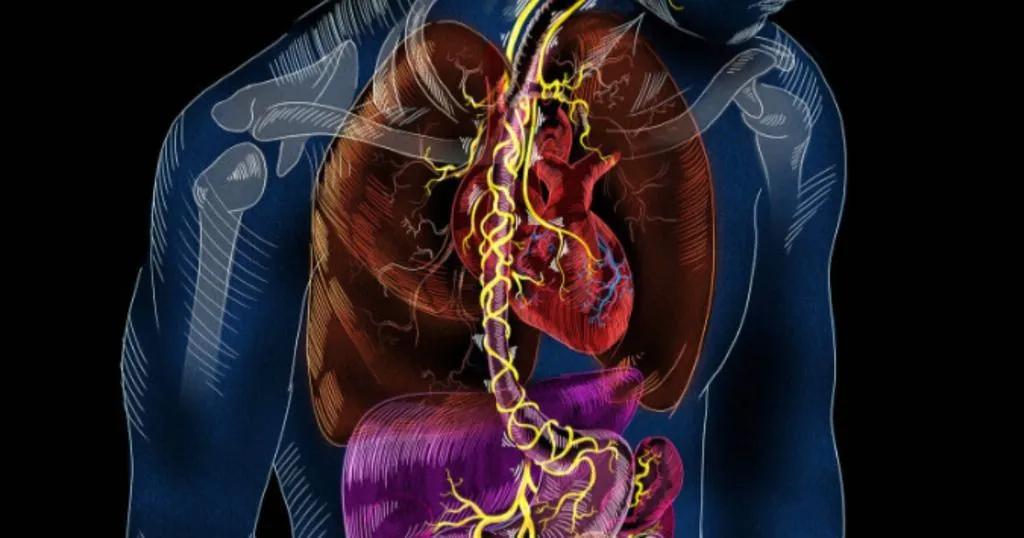
The question is, how were these signals transmitted? To find out, the researchers removed the vagus nerve from the mice that had received the fecal transplants. The vagus nerve is a critical communication pathway between the brain and various organs, including the digestive system. Once the nerve was removed, the transplanted mice no longer showed signs of depression, indicating that the vagus nerve was the key pathway transmitting signals from the gut to the brain.
What does the Vagus nerve do?
The vagus nerve has about 200,000 fibers connecting the brain to major organs like the heart, lungs, and digestive tract. It controls many bodily functions, such as heart rate, digestion (by managing peristalsis), and even signals satiety—telling you when you’ve eaten enough. In this case, the nerve was acting as a conduit for stress signals from the gut to the brain.

Image from sayostudio.com (Science Communication)
Neurotransmitter disruption in the Brain
The researchers also examined the brains of the fecal transplant mice and discovered that key neurotransmission pathways for serotonin and dopamine were impaired. Serotonin plays a major role in mood regulation, cognition, and learning, while dopamine is essential for motivation and reward-based behaviors. Disruptions in these systems explained why the mice exhibited depression-like symptoms.
So, what did we learn?
In summary, if the gut flora of a ‘depressed’ mouse is transplanted to another mouse, that mouse will also show symptoms of depression. That works by transmission of a signal from the gut to the brain by the vagus nerve. This study thus reveals that gut bacteria can directly influence brain function to the extent that symptoms of stress and depression can indeed be transferred between individuals. The gut and brain truly are very closely linked, the next time you think about mental well-being, remember that it may just start in your gut.
References
[1] Siopi, E., Galerne, M., Rivagorda, M. et al. Gut microbiota changes require vagus nerve integrity to promote depressive-like behaviors in mice. Mol Psychiatry 28, 3002–3012 (2023). https://doi.org/10.1038/s41380-023-02071-6
Related Posts

Is a unique calcium regulating mechanism a cause of Gulf War Illness?

Fearful chicken: Fear affects stress, behavior patterns, and other individuals


