The challenges of measuring epilepsy in rodents
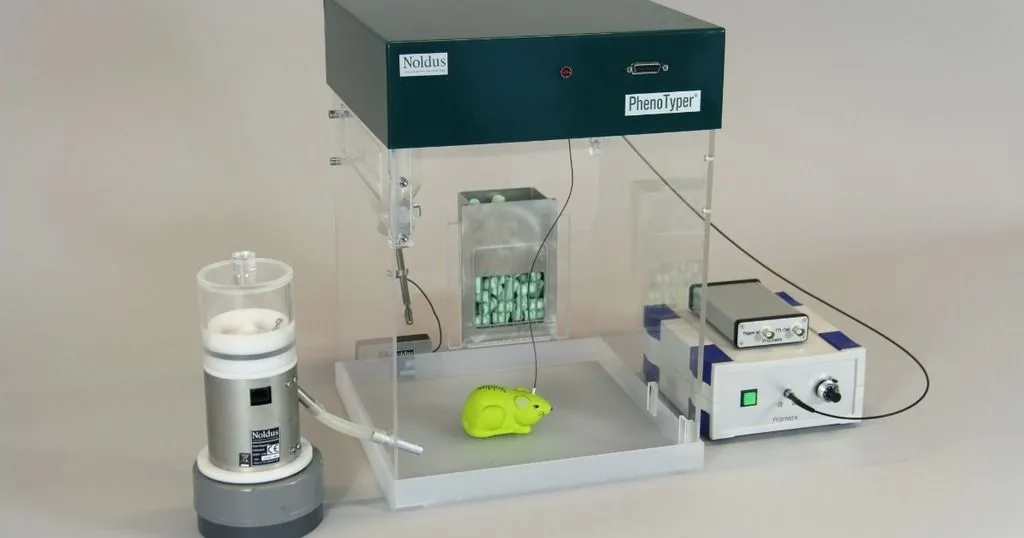
EEG on freely moving rats? It's possible in the PhenoTyper. This was necessary to measure if delivering drugs directly to the brain could help epilepsy patients.
Posted by
Published on
Thu 30 Mar. 2023
Topics
| EthoVision XT | PhenoTyper | Seizure Behavior | Epilepsy |
What is epilepsy?
Epilepsy is a disease (actually, a group of disorders) in which the patients experience a large synchronous discharge of electrical discharge in their brains - a seizure. Seizures often cause convulsive muscle contractions, which can cause accidents, broken bones and bitten tongues. (Here is what to do if you see someone having a seizure).
Sometimes the seizure causes absences, in which the patient has decreased levels of consciousness. Those typically last about ten seconds, but it can be much longer. Epilepsy has a variety of causes include genetics (typically in younger people), brain trauma, and stroke (typically in older people).
The blood brain barrier
Over fifty million people worldwide suffer from epilepsy. Although there are working drugs, which can help most epilepsy patients, about 30% of patients cannot be helped by current medicines. One of the reasons for that is that the brain has a mechanism called the blood brain barrier (BBB) to protect it.
The BBB is a wall of cells which selectively prevents bacteria, viruses and chemicals in the blood from getting into the central nervous systems (the brain and spinal cord). Chemicals like oxygen and hormones are allowed through the barrier or are actively transported, for example glucose as 'fuel' for the brain.
The BBB is a powerful mechanism defending the brain, but it does result in medicines intended to alleviate diseases like epilepsy to be prevented or restricted from getting to the brain. If a higher dose of the medicine is given, so that enough gets through to help the patient, that can cause all sorts of negative effects in other organs of the body.
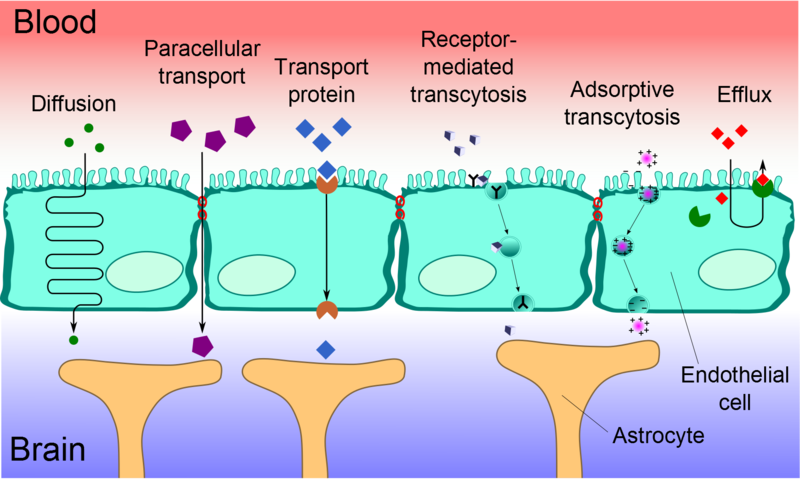
Diagram of the function of the blood brain barrier (Wikimedia Commons).
Injecting directly into the brain
An alternative is to inject medicines directly into the brain. Specifically, they can be injected into the cerebrospinal fluid in the cerebral ventricels (intracerebroventricular administration, i.c.v.). The cerebral ventricles are cavities in the brain that produce the cerebrospinal fluid. Cerebrospinal fluid is a clear liquid found in the brain and spinal cord of vertebrates, which provides mechanical and immunological protection.
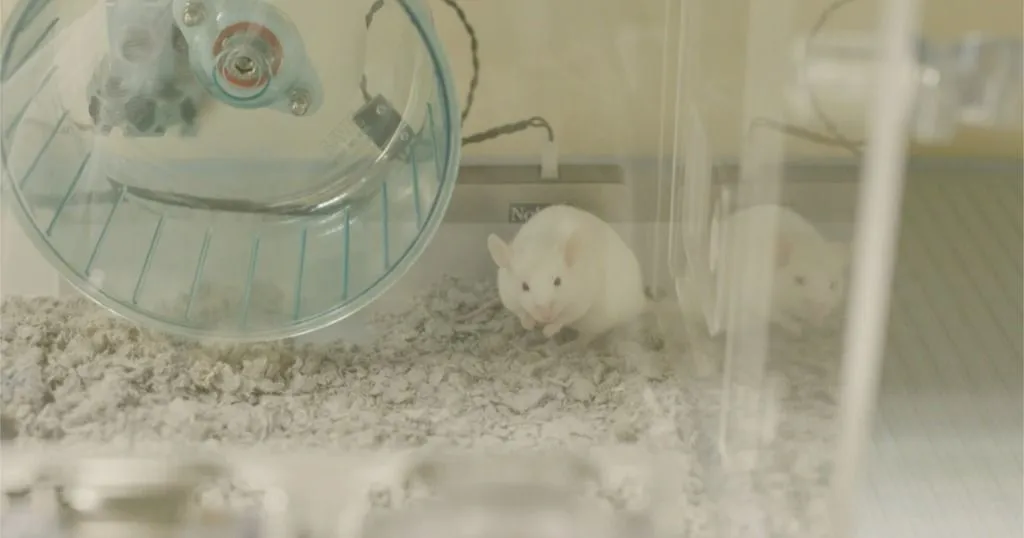
However, until recently, it wasn't known if this i.c.v. injection was likely to work. Anna-Sophia Buschhoff and her colleagues [1] in Kiel University (Germany) investigated this using a special variety of rat, with a genetic disposition to having epileptic seizures: the Genetic Absence Epilepsy Rats from Strasbourg (GAERS).
Measuring behavior with the PhenoTyper
The researchers implanted a thin polythene tube into one of the ventricles of the rat's brains (an i.c.v. cannula) and injected them with ethosuximde (ETX). ETX is a medicine widely used to treat epileptic patients to reduce seizures. They monitored if there were any abnormal behaviors by observing the rats in an open field (no such behaviors were observed) and measured the electrical activity of the rat's brains (EEG) to monitor spike wave discharges (electrical activity that leads to seizures).
That was easier said than done, the EEG headstages needed to be connected to recording equipment by a cable, but the rats also needed to have freedom of movement so that they could behave normally.
This problem was solved by using a PhenoTyper from Noldus IT. The PhenoTyper is an instrumented cage which can facilitate the measuring of the behavior of laboratory rats and mice, but it also has the possibility to attach cables to a swivel so that the rats could move freely. In this case, it was an electrical swivel with a counterbalanced arm, so that the rats' heads could also move up and down.
The behavior of the rats was also monitored using EthoVision XT. The effects were compared with i.c.v. injections and injections into the tail vein, and at various different dosages (including a control with no ETX).
Direct injection in the brain reduces seizures
The results were quite spectacular. In the rats which had ETX injected through the tail vein, there was no reduction in spike wave discharges. However, in the rats which had i.c.v. injections of ETX into the brain, there was a strong reduction in spike waves and seizures, and also fewer convulsions, even at low doses.
Treating epilepsy in humans
Of course, for human patients, injection of a drug via a cannula into the brain is not a very appealing prospect. However, there are some better possibilities, which are currently being researched:
- The drugs could be combined with a molecule that the blood brain barrier does let through.
- Drugs could also be used to increase the permeability of the BBB (though that is a risky procedure that can only be carried out in controlled circumstances).
- The most promising route is to attach the medicine to coated nanoparticles, which can get through the BBB [2].
For some of the millions of epilepsy patients who cannot be helped with current medical techniques, these innovations might make a huge difference to their lives in the future.
References
1. Anna-Sophia Buschhoff, Regina Scherließ, Johanne G. de Mooij-van Malsen, Thomas Schiffelholz, Ulrich Stephani, Peer Wulff, (2022). Intrathecal application of ethosuximide is highly efficient in suppressing seizures in a genetic model of absence epilepsy. Epilepsy Research 184, 106967. https://doi.org/10.1016/j.eplepsyres.2022.106967.
2. Dadparvar, M., Wagner, S., Wien, S., Kufleitner, J., Worek, F., von Briesen, H., & Kreuter, J. (2011). HI 6 human serum albumin nanoparticles—Development and transport over an in vitro blood–brain barrier model. Toxicology Letters, 206(1), 60-66. doi:10.1016/j.toxlet.2011.06.027
Related Posts

Behavioral research shows how elephants like their new habitat at the Oregon Zoo
Home cage behavior and epilepsy in the Stargazer mutant mouse

